Top Stories
Researchers Unveil Light-Based Cancer Treatment to Replace Chemotherapy
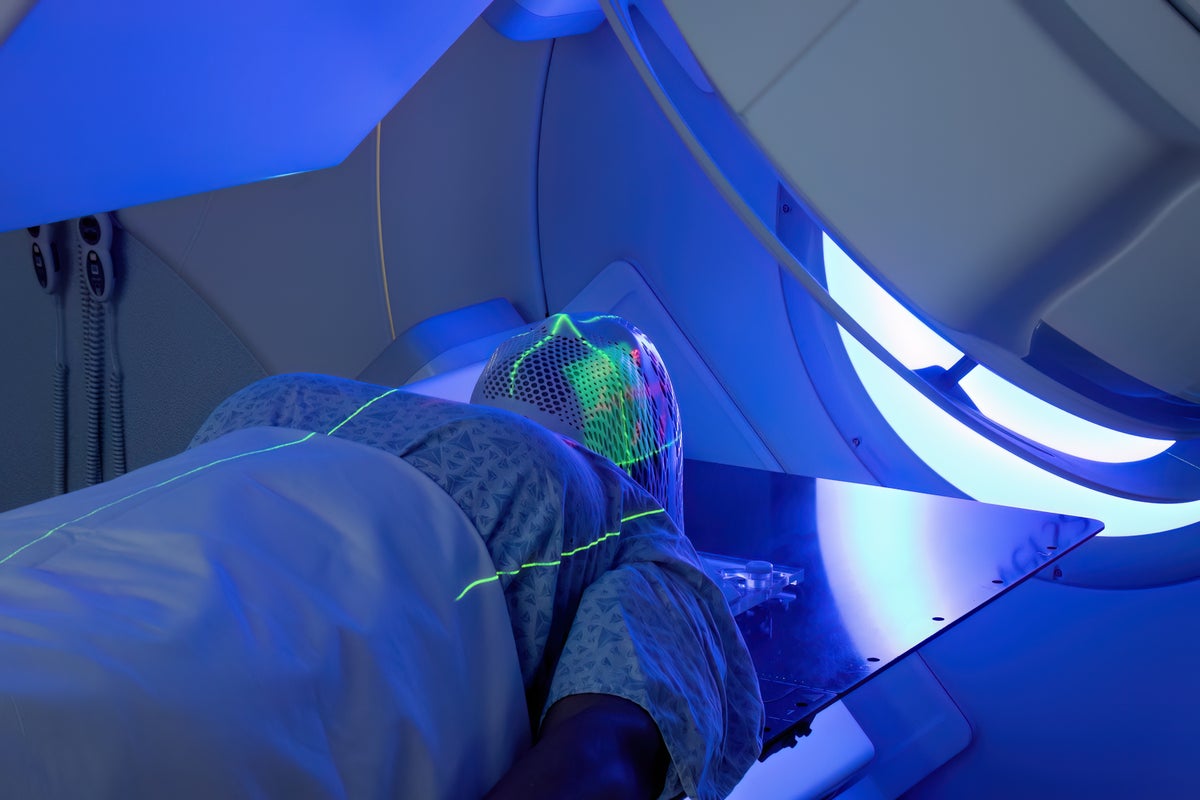
A new light-based treatment developed by researchers in the United States has the potential to offer a safer alternative to traditional chemotherapy. This innovative approach combines near-infrared LED light with nanoscopic flakes of tin oxide, known as SnOx nanoflakes, to target and destroy cancer cells while sparing healthy tissues. This advancement could significantly change the landscape of cancer therapy by minimizing the severe side effects commonly associated with chemotherapy and radiotherapy.
The treatment is rooted in the principles of photothermal therapy, which utilizes light to generate heat that specifically targets tumours. Unlike conventional methods that often employ expensive lasers, this new technique relies on affordable and accessible LED systems. This shift not only reduces damage to surrounding healthy tissue but also provides a more viable option for clinical use, including potential at-home applications.
At the heart of this innovation is the ability to create localized heat through the absorption of near-infrared light by the SnOx nanoflakes. When exposed to this light, the nanoflakes effectively function as tiny heaters, generating sufficient warmth to disrupt the membranes and proteins of cancer cells, ultimately leading to cell death. Healthy cells remain largely unaffected because they are less sensitive to heat and the nanoflakes can be directed specifically to malignant cells.
In laboratory studies, this combination has demonstrated remarkable efficacy, destroying up to 92 percent of skin cancer cells and 50 percent of colorectal cancer cells within just 30 minutes. Importantly, healthy human skin cells showed no adverse effects, making this technique particularly promising for treating cancers such as melanoma and basal cell carcinoma, which can be effectively targeted by light exposure.
The researchers developed the SnOx nanoflakes from tin disulfide (SnS2), converting it into oxygenated tin oxide. This transformation enhances the nanoflakes’ ability to absorb near-infrared light, which can safely penetrate biological tissues. Furthermore, the production process is non-toxic and sustainable, eliminating harmful solvents and expensive manufacturing steps.
The team envisions a future where compact LED devices could be applied directly to the skin post-surgery, allowing for the destruction of any remaining malignant cells and reducing the risk of cancer recurrence. For example, following the removal of a melanoma or basal cell carcinoma, a patch-like LED device could deliver focused light to activate the nanoflakes at the surgical site, creating a safer and more convenient option for post-surgical cancer care.
This innovation may also pave the way for combination therapies. By weakening cancer cells, photothermal treatment can enhance the effectiveness of other therapies, such as immunotherapy or targeted drugs. The heat generated may trigger immune responses that help the body identify and eliminate cancer cells, leading to a more comprehensive treatment approach.
As research progresses, the team is further refining the technology. They are investigating how different wavelengths and exposure times impact treatment outcomes and exploring the potential of alternative materials that could penetrate deeper tissues, such as those affected by breast or colorectal cancers.
Another exciting avenue of research includes the development of implantable nanoflake systems, which could provide ongoing photothermal control within the body. The accessibility of LED-based devices stands out as a significant advantage. Given their low manufacturing cost and ease of use, these devices could be deployed in low-resource regions with limited access to cancer care, democratizing advanced treatment options.
For superficial cancers detected early, LED therapy might even be integrated into outpatient or cosmetic procedures, reducing recovery time and enhancing patients’ quality of life. Additionally, the safety profile of photothermal therapy is compelling. Unlike chemotherapy, which damages rapidly dividing healthy cells throughout the body, this targeted approach confines its effects to the illuminated site, producing minimal discomfort and avoiding systemic toxicity.
The promising results observed in laboratory settings are a stepping stone toward preclinical and, ultimately, human trials. While challenges remain, LED-driven photothermal therapy may redefine cancer treatment, making it more precise, affordable, and humane. As researchers continue to innovate, the vision of non-invasive, localized, patient-friendly cancer therapies is becoming increasingly tangible.
-

 World2 weeks ago
World2 weeks agoCoronation Street’s Shocking Murder Twist Reveals Family Secrets
-

 Entertainment1 week ago
Entertainment1 week agoAndrew Pierce Confirms Departure from ITV’s Good Morning Britain
-

 Entertainment5 months ago
Entertainment5 months agoKate Garraway Sells £2 Million Home Amid Financial Struggles
-

 Entertainment4 months ago
Entertainment4 months agoAnn Ming Reflects on ITV’s ‘I Fought the Law’ Drama
-
 Entertainment1 month ago
Entertainment1 month agoCoronation Street Fans React as Todd Faces Heartbreaking Choice
-

 Health4 months ago
Health4 months agoKatie Price Faces New Health Concerns After Cancer Symptoms Resurface
-

 World1 month ago
World1 month agoBailey Announces Heartbreaking Split from Rebecca After Reunion
-

 Entertainment2 weeks ago
Entertainment2 weeks agoTwo Stars Evicted from I’m A Celebrity Just Days Before Finale
-

 World2 weeks ago
World2 weeks agoKevin Sinfield Exceeds Fundraising Goal Ahead of Final Marathons
-

 Entertainment4 months ago
Entertainment4 months agoCoronation Street’s Carl Webster Faces Trouble with New Affairs
-

 Entertainment4 months ago
Entertainment4 months agoWhere is Tinder Swindler Simon Leviev? Latest Updates Revealed
-

 Entertainment5 months ago
Entertainment5 months agoMarkiplier Addresses AI Controversy During Livestream Response





















