Health
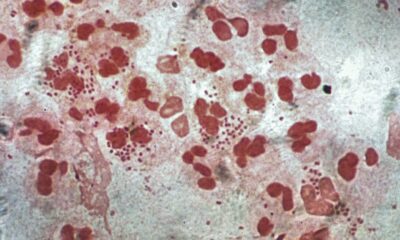
Researchers Uncover New Pathways in Staph Bacteria’s Survival Tactics
Researchers from Michigan State University (MSU) have made a significant discovery regarding the survival mechanisms of Staphylococcus aureus, commonly known as staph. Their study reveals that staph bacteria possess a surprising level of metabolic redundancy, which may influence how deadly pathogens are targeted in the ongoing fight against antibiotic resistance.
Staph infections, while often harmless, can escalate into serious health threats. A notable strain, methicillin-resistant Staphylococcus aureus (MRSA), is resistant to many commonly used antibiotics, complicating treatment options. The findings from this research, published in the journal mBio, suggest potential new avenues for antibiotic development.
Understanding Metabolic Redundancy in Staph
Led by recently graduated PhD student Troy Burtchett from MSU’s Department of Microbiology, Genetics, and Immunology, the research highlights the role of isoprenoids—molecules vital for bacterial survival. These compounds are involved in various functions, including pigment production, respiration, and cell wall synthesis.
Traditionally, the enzyme IspA was thought to be the sole producer of short-chain isoprenoids. However, Burtchett and his team discovered that when they created staph mutants lacking the gene ispA, the bacteria continued to thrive. This unexpected outcome prompted further investigation into how staph could tolerate the mutation.
Burtchett explained, “How can the cell tolerate that? That’s really what started this project off. It was really just a basic science investigation.”
In collaboration with Neal Hammer, an associate professor at MSU, and doctoral student Jessica Lysne, the researchers investigated another enzyme, HepT, which was found to be compensating for the loss of IspA. This led to the conclusion that HepT is involved in pathways not previously recognized, including the synthesis of molecules essential for respiration.
Implications for Antibiotic Development
To test their hypothesis, the team engineered a double mutant lacking both ispA and the corresponding gene for HepT. Surprisingly, the bacteria remained viable, indicating the existence of a third, unidentified enzyme that compensates for the loss of the other two. Burtchett noted, “One of the conclusions is that there is an incredible level of redundancy in isoprenoid synthesis in S. aureus. This has never been demonstrated before.”
These findings could have broader implications as isoprenoid synthesis pathways are highly conserved across various bacterial species. The research suggests that similar mechanisms might apply to other pathogens, including E. coli and Pseudomonas.
The rise of antibiotic resistance poses a significant challenge in medicine, as bacteria continue to evolve ways to resist treatment. By identifying new metabolic pathways that have not been targeted previously, researchers hope to develop antibiotics that bacteria have not yet developed defenses against. Burtchett stated, “If it’s new, there’s probably not existing resistance to it, and you can get more use out of that antibiotic.”
Looking forward, the team aims to further explore these findings to identify the third short-chain isoprenoid synthesis enzyme. Hammer emphasized, “Identifying this enzyme will provide new targets for therapeutic intervention,” potentially paving the way for innovative treatments against antibiotic-resistant infections.
The research was supported by a grant from the National Institutes of Health (NIH), underscoring the importance of this work in the global fight against antibiotic resistance. The findings not only contribute to the scientific community’s understanding of bacterial survival strategies but also offer hope for future drug discovery efforts.
-

 Entertainment3 months ago
Entertainment3 months agoAnn Ming Reflects on ITV’s ‘I Fought the Law’ Drama
-

 Entertainment4 months ago
Entertainment4 months agoKate Garraway Sells £2 Million Home Amid Financial Struggles
-

 Health3 months ago
Health3 months agoKatie Price Faces New Health Concerns After Cancer Symptoms Resurface
-

 Entertainment3 months ago
Entertainment3 months agoCoronation Street’s Carl Webster Faces Trouble with New Affairs
-

 Entertainment3 months ago
Entertainment3 months agoWhere is Tinder Swindler Simon Leviev? Latest Updates Revealed
-

 Entertainment4 months ago
Entertainment4 months agoMarkiplier Addresses AI Controversy During Livestream Response
-

 Science1 month ago
Science1 month agoBrian Cox Addresses Claims of Alien Probe in 3I/ATLAS Discovery
-

 Health4 months ago
Health4 months agoCarol Vorderman Reflects on Health Scare and Family Support
-

 World2 weeks ago
World2 weeks agoBailey Announces Heartbreaking Split from Rebecca After Reunion
-

 Entertainment4 months ago
Entertainment4 months agoKim Cattrall Posts Cryptic Message After HBO’s Sequel Cancellation
-

 Entertainment3 months ago
Entertainment3 months agoOlivia Attwood Opens Up About Fallout with Former Best Friend
-
 Entertainment2 weeks ago
Entertainment2 weeks agoCoronation Street Fans React as Todd Faces Heartbreaking Choice